Table of Contents
- Lipedema Reduction Surgery Improves Pain, Mobility, Physical Function, and Quality of Life: Case Series Report
- Real time visualization of enhanced lymphatic flow when using a non-pneumatic active compression device (NPCD)
- Effect of pneumatic compression device and stocking use on symptoms and quality of life in women with lipedema: A proof-in-principle randomized trial
- A Case Series of Lymphatic Injuries After Suction Lipectomy in Women with Lipedema
- A Young Woman with Excessive Fat in Lower Extremities Develops Disordered Eating and Is Subsequently Diagnosed with Anorexia Nervosa, Lipedema, and Hypermobile Ehlers-Danlos Syndrome
- Standard of care for lipedema in the United States
- Survey Outcomes of Lipedema Reduction Surgery in the United States, Plastic and Reconstructive Surgery
- A 41-Year-Old Woman with Excessive Fat of theLower Body Since Puberty with Progression to Swollen Ankles and Feet Despite Caloric Restriction, Due to Lipedema and Protein-Calorie Malnutrition: A Case of Stage 3 Lipedema
- Lipedema Fat and BMI
- Lipedema – A Devastating Disease too Often Overlooked
Lipedema Reduction Surgery Improves Pain, Mobility, Physical Function, and Quality of Life: Case Series Report
Real time visualization of enhanced lymphatic flow when using a non-pneumatic active compression device (NPCD)
Effect of pneumatic compression device and stocking use on symptoms and quality of life in women with lipedema: A proof-in-principle randomized trial
A Case Series of Lymphatic Injuries After Suction Lipectomy in Women with Lipedema
4. Thomas F. Wright, Karen L. Herbst. A Case Series of Lymphatic Injuries After Suction Lipectomy in Women with Lipedema. Am J Case Rep Accepted June 4 , 2022 Wright TF, Herbst KL. A Case Series of Lymphatic Injuries After Suction Lipectomy in Women with Lipedema. Am J Case Rep. 2022 Jul 11;23:e935016. doi: 10.12659/AJCR.935016. PMID: 35811389; PMCID: PMC9284075. https://pubmed.ncbi.nlm.nih.gov/35811389/
A Young Woman with Excessive Fat in Lower Extremities Develops Disordered Eating and Is Subsequently Diagnosed with Anorexia Nervosa, Lipedema, and Hypermobile Ehlers-Danlos Syndrome
5. Wright TF, Herbst KL. A Young Woman with Excessive Fat in Lower Extremities Develops Disordered Eating and Is Subsequently Diagnosed with Anorexia Nervosa, Lipedema, and Hypermobile Ehlers-Danlos Syndrome. Am J Case Rep. 2021 Jun 14;22:e930840. doi: 10.12659/AJCR.930840. PMID: 34121088. https://library.lipedema.org/bibliography/JUPHV8G3
Standard of care for lipedema in the United States
6.Herbst KL, Kahn LA, Iker E, Ehrlich C, Wright T, McHutchison L, Schwartz J, Sleigh M, Donahue PM, Lisson KH, Faris T, Miller J, Lontok E, Schwartz MS, Dean SM, Bartholomew JR, Armour P, Correa-Perez M, Pennings N, Wallace EL, Larson E. Standard of care for lipedema in the United States. Phlebology. 2021 May 28:2683555211015887. doi: 10.1177/02683555211015887. PMID: 34049453. https://journals.sagepub.com/doi/10.1177/02683555211015887
Survey Outcomes of Lipedema Reduction Surgery in the United States, Plastic and Reconstructive Surgery
7.Herbst, Karen L. PhD, MD*, †, ∥; Wright, Thomas F. MD§; Larson, Ethan E. MD; Schwartz, Jaime S. MD, FACS∥,** Survey Outcomes of Lipedema Reduction Surgery in the United States, Plastic and Reconstructive Surgery – Global Open: April 2021 – Volume 9 – Issue 4 https://www.lipedema.net/survey-outcomes-of-lipedema-reduction-surgery.html https://www.lipedema.net/survey-outcomes-of-lipedema-reduction-surgery.html
A 41-Year-Old Woman with Excessive Fat of theLower Body Since Puberty with Progression to Swollen Ankles and Feet Despite Caloric Restriction, Due to Lipedema and Protein-Calorie Malnutrition: A Case of Stage 3 Lipedema
Lipedema Fat and BMI
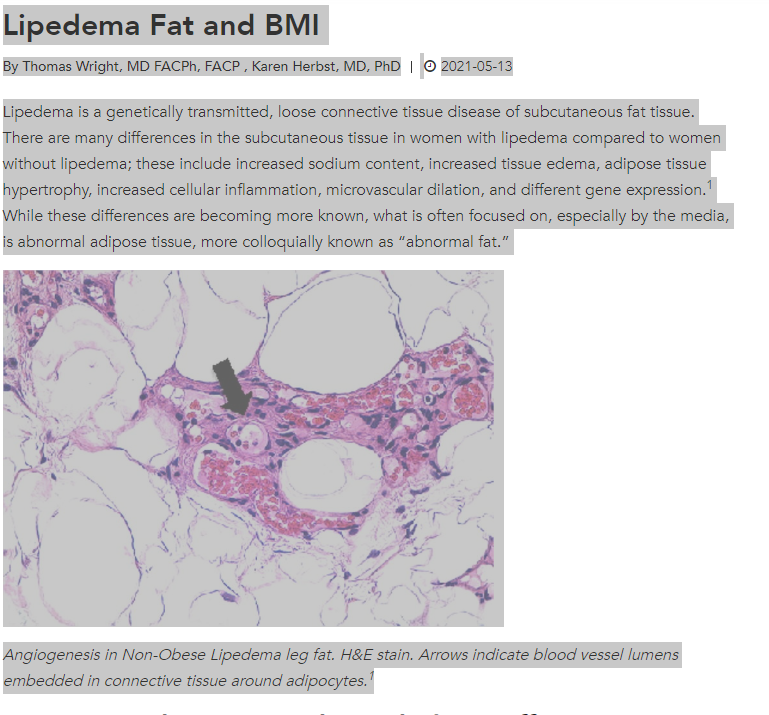
9.Wright T, Herbst K., Lipedema Fat and BMI. Vein Magazine. Fall 2021. Online 5-13-21. https://www.veindirectory.org/magazine/article/techniques-technology/lipedema-fat-and-bmi
Lipedema – A Devastating Disease too Often Overlooked
by Dr. Thomas Wright for the Vein Magazine

